In patients with anterior shoulder instability, understanding the nature and extent of a Bony Bankart lesion is critical for effective management. Classification systems and precise measurement of the glenoid bone loss help determine whether nonoperative care, arthroscopic repair, or bony augmentation is needed. This article explores how lesion size is assessed and the key thresholds used to categorize bone loss severity.
1. What Is a Bony Bankart Lesion?
A Bony Bankart lesion is an avulsion of the anteroinferior labrum along with a segment of the glenoid rim. It usually results from traumatic anterior shoulder dislocations and contributes to recurrent instability if not properly addressed.
2. Importance of Lesion Classification
Why Classification Matters
- Guides surgical decision-making
- Predicts risk of recurrence
- Helps determine need for augmentation procedures like Latarjet
Common Classification Criteria
- Fragment size (absolute and relative to glenoid surface)
- Displacement and rotation of fragment
- Chronicity (acute vs chronic appearance on imaging)
- Engagement with humeral head defect (Hill–Sachs)
3. Methods of Measuring Bone Loss
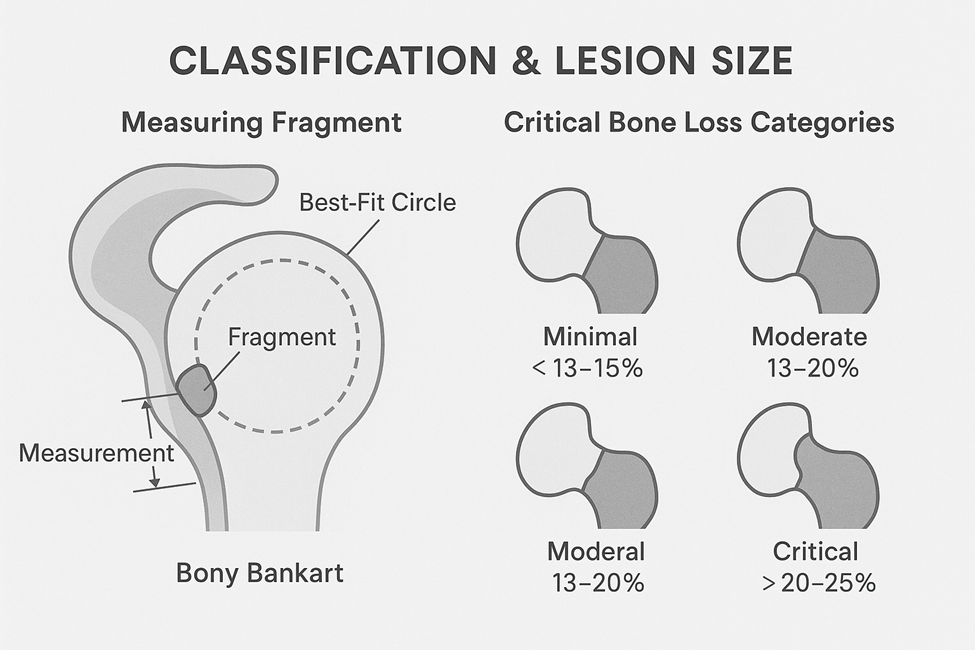
3.1 Best-Fit Circle Method
- CT or MR arthrography is used to draw a perfect circle encompassing the intact glenoid.
- Missing bone along the anterior-inferior rim is measured as a linear or arc segment.
- Bone loss is calculated as a percentage of the original glenoid diameter or area.
3.2 Surface Area Assessment
- 3D reconstruction software allows comparison of affected glenoid to the contralateral (normal) side.
- Quantifies percentage of surface area lost.
3.3 Glenoid Track Concept
- Assesses whether the Hill–Sachs lesion stays within the glenoid track during arm movement.
- If it engages outside this zone, it is deemed “off-track” and often necessitates bone grafting or Latarjet procedure.
4. Classification by Bone Loss Severity
Minimal (<13–15%)
- Often treated with arthroscopic Bankart repair alone
- Stability restored without augmentation
- Good prognosis
Moderate (13–20%)
- May still be amenable to arthroscopic repair
- Close monitoring required for re-dislocation risk
- Consideration for individualized treatment based on activity level
Critical (>20–25%)
- Associated with high recurrence after soft tissue repair
- Requires bony augmentation (e.g., Latarjet or iliac crest bone graft)
- Associated with the inverted pear glenoid—a visual cue of significant bone loss
5. Classification Systems in Use
5.1 Sugaya Classification
- Based on CT imaging
- Type I to V depending on fragment size, healing, and remodeling
- Helps determine chronicity and healing potential
5.2 Shaha Classification
- Focuses on glenoid shape and bone loss using en face 3D CT images
- Grades the glenoid based on volume and rim integrity
6. Clinical Implications of Lesion Size
6.1 Predicting Surgical Outcomes
- Soft tissue repairs in the presence of unrecognized critical bone loss have higher failure rates.
- CT-based measurement improves preoperative planning accuracy.
6.2 Choosing the Right Surgery
- Arthroscopic Bankart repair: Small bone loss, minimal symptoms
- Open Latarjet or bone block: Large fragment or critical loss
- Remplissage: For engaging Hill–Sachs lesions, often in combination with glenoid procedures
FAQs
1. What is considered critical bone loss in a Bony Bankart lesion?
Typically, loss of ≥20–25% of the glenoid surface is considered critical and indicates the need for bone augmentation.
2. Can MRI alone measure bone loss accurately?
MRI can give an estimate, but CT—especially with 3D reconstructions—is the gold standard for accurate bone loss measurement.
3. Is the inverted pear glenoid a reliable sign?
Yes, it visually represents significant bone loss and correlates with the threshold requiring surgical augmentation.
4. Do all patients with Bony Bankart need surgery?
Not necessarily. If the bone loss is minimal and instability is controlled, nonoperative or soft tissue repair may suffice.
5. How often should lesion size be reassessed?
Once identified, reassessment is generally only needed if symptoms worsen, or in the context of revision surgery planning.
Conclusion
Proper classification and measurement of Bony Bankart lesions are vital in guiding treatment. Using objective methods like the best-fit circle technique and 3D CT imaging helps identify whether a lesion falls into the critical bone loss category. Recognizing these patterns early can prevent failed repairs and optimize surgical outcomes.
