Athletes place extraordinary demands on their shoulders. When instability occurs—often linked to Bony Bankart lesions—it can threaten both performance and career longevity. Managing these injuries requires an understanding of sport‑specific risks, tailored treatment, and realistic return‑to‑play timelines. Let’s dive into how these factors shape care for athletes.
1. Why Athletes Are at Higher Risk
Repetitive Stress and High Forces
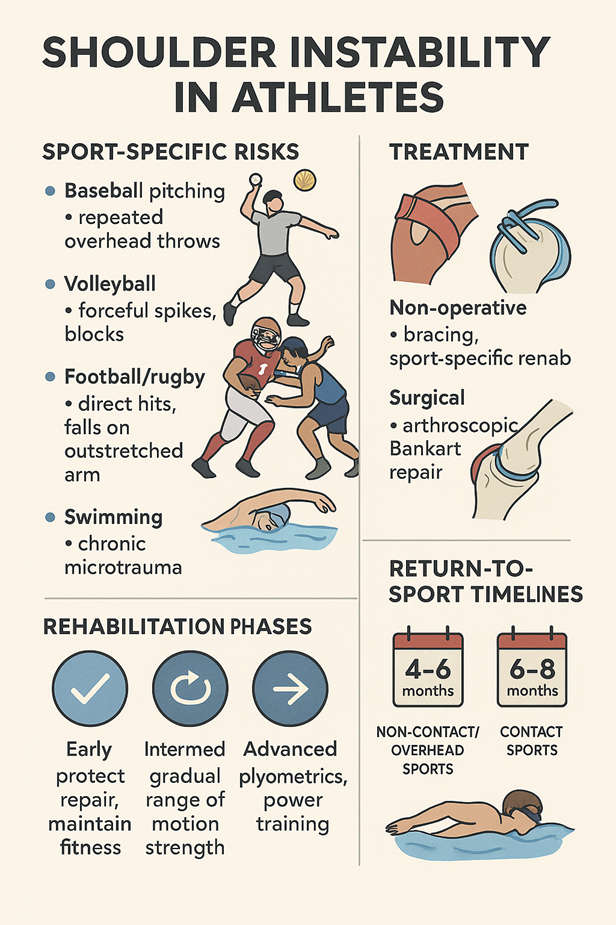
- Overhead sports (e.g., baseball, volleyball, swimming) subject the shoulder to extreme external rotation and torque, predisposing to labral and bony injuries.
- Contact sports (e.g., football, rugby, wrestling) expose the shoulder to direct trauma and dislocation events.
Hyperlaxity and Prior Injuries
- Many athletes have naturally looser joints, offering performance advantages but increasing instability risk.
- Previous subluxations or dislocations compound the risk of further damage.
2. Sport‑Specific Patterns
| Sport | Common Mechanism | Key Concerns |
| Baseball Pitching | Repeated overhead throws | Labral attrition, subtle bone loss, velocity decline |
| Volleyball | Forceful spikes, blocks | High stress in extreme external rotation |
| Football/Rugby | Direct hits, falls on outstretched arms | Large fragments, recurrent dislocations |
| Swimming | Chronic microtrauma | Capsular laxity, labral wear |
3. Diagnosis and Imaging in Athletes
- Early MRI/MR Arthrography: Detects subtle soft‑tissue injuries that could worsen under continued play.
- CT with 3D Reconstructions: Essential if bony involvement is suspected.
- Dynamic Physical Examination: Recreates sport‑specific positions to assess instability and apprehension.
4. Treatment Strategies
Non‑Operative in Selected Cases
- Indicated For: Minimal bone loss, low‑demand phases of season, and athletes willing to modify activity.
- Approach: Bracing during play, targeted rehab focusing on scapular stability and rotator cuff strength.
Surgical Management
- Arthroscopic Bankart Repair: Preferred for athletes with minimal to moderate bone loss seeking rapid recovery.
- Latarjet Procedure: Reserved for critical bone loss (>20–25%) or failed prior repairs, particularly in contact sports.
5. Rehabilitation Considerations for Athletes
Early Phase
- Protect repair while maintaining cardiovascular fitness.
- Emphasize scapular kinematics and controlled ROM.
Intermediate Phase
- Integrate sport‑specific motions gradually.
- Monitor for apprehension or residual laxity during simulated movements.
Advanced Phase
- Plyometric and power exercises mimicking sport demands.
- Return‑to‑throw or hitting programs with incremental workload increases.
6. Return‑to‑Sport Timelines
- Non‑contact, overhead sports: Typically return around 4–5 months post‑repair if strength and ROM benchmarks are met.
- Contact sports: Often delayed to 6–8 months, ensuring robust healing and stability under impact.
- Performance metrics: Functional tests, fatigue assessments, and confidence questionnaires guide final clearance.
7. Performance Outcomes
- Stability: Most athletes achieve long‑term stability with appropriate treatment.
- Performance: Studies show return to preinjury performance levels in 80–90% of cases after arthroscopic repair.
- Longevity: Proper care reduces recurrent instability and protects career duration.
FAQs
1. Can athletes continue their season after a first dislocation?
In some cases, yes—if bone loss is minimal and bracing plus rehab are effective. However, recurrence risk remains.
2. Does surgery guarantee a full return to sport?
While outcomes are excellent, individual factors like bone loss and sport type influence results.
3. How soon can throwing drills begin post‑repair?
Typically around 3 months, starting with light tosses and progressing under supervision.
4. Are contact sports more likely to need surgery?
Yes, due to higher rates of bony injury and recurrent dislocation risk.
5. Do athletes regain their preinjury strength?
Most do, provided they complete a comprehensive rehab program tailored to their sport.
Shoulder instability in athletes demands a nuanced approach that balances immediate performance goals with long‑term joint health. By understanding sport‑specific risks, employing the right treatment strategy, and following structured rehabilitation, most athletes not only return to their sport but also regain confidence and durability in their shoulder.
