The shoulder joint ranks among the most mobile yet complex joints in the human body. Central to its stability is the glenoid—the shallow, pear-shaped part of the scapula that forms the socket for the head of the humerus. This article explores the detailed anatomy and biomechanics of the glenoid, with a particular focus on the glenoid rim: how it contributes to joint stability and what happens when this structure is fractured, such as in a Bony Bankart lesion.
1. Anatomy of the Glenoid
1.1. Basic Structure
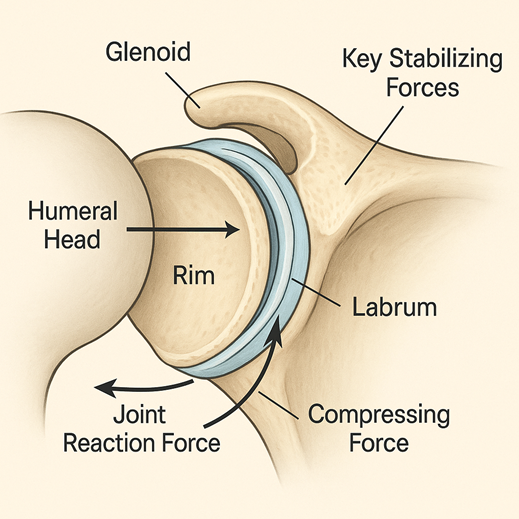
- Glenoid Fossa: A concave surface on the lateral edge of the scapula where the humeral head articulates.
- Glenoid Labrum: A fibrocartilaginous ring that deepens the fossa by about 50%, reinforcing joint stability.
- Glenoid Rim: The peripheral margin just outside the labrum that adds a bony stop against anterior or inferior displacement.
1.2. Glenoid Orientations and Dimensions
- Vertical Orientation: Slightly inclined upward; prevents excessive downward translation.
- Horizontal Tilt: About 8–15° retroverted to align with the humeral head.
- Surface Area: Small; yet compensated by precise articulating congruence, ensuring stability during movement.
1.3. Vascular and Nerve Supply
- Supplied primarily by branches of the suprascapular, circumflex scapular, and dorsal scapular arteries.
- Innervation from suprascapular and axillary nerves, which also support proprioception.
2. Biomechanics: How the Glenoid Rim Stabilizes the Shoulder
2.1. Static Stabilizers
- Bony Congruence: The labrum and rim concentric structure serve as a physical barrier.
- Labral Seal (Suction Effect): The deepening effect of the labrum creates negative intra-articular pressure, pulling the humeral head into the socket.
2.2. Dynamic Stabilizers
- Rotator Cuff Muscles: Supraspinatus, infraspinatus, teres minor, and subscapularis provide constant compressive forces across the joint.
- Periscapular Muscles: Scapular stabilizers (trapezius, serratus anterior) maintain optimal glenoid orientation.
2.3. Force Transmission & Load Distribution
- Compression: During movement (e.g., lifting arms), compressive loads are transmitted to the glenoid.
- Shear Forces: Anteriorly directed forces during abduction/external rotation are resisted by the labrum and rim.
- Edge Loading: Minor rim irregularities are tolerated, but rim loss or fractures significantly increase stress on soft tissues.
3. Glenoid Rim Fractures: Impact on Shoulder Mechanics
3.1. Typical Mechanism of Injury
- Caused by an anterior shoulder dislocation, particularly when the arm is abducted and externally rotated.
- The humeral head collides with the anteroinferior rim, creating a fracture in the bone and sometimes damaging the labrum.
3.2. Size of Fragment Matters
- < 13–20% rim involvement: Tightens the adhesive labral seal, but joint often maintains reasonable stability.
- > 20–25% loss: Leads to severe instability, recurrent dislocations, and altered biomechanics.
3.3. Glenoid Version Alteration
- Rim loss changes the orientation of the socket—usually becoming more anteverted—allowing abnormal anterior translation over time.
4. Diagnostic Evaluation of Glenoid Rim Integrity
4.1. Imaging Studies
- 2D/3D CT Scans: Provide accurate measurement of bony loss and realignment assessments.
- MRI (with or without Arthrogram): Highlights labral tears and soft tissue damage adjacent to bone fragments.
4.2. Clinical Tests
- Apprehension Test: Elicits fear of dislocation in the abducted and externally rotated position.
- Relocation Test: Ease of pain on applying posterior pressure confirms anterior laxity.
- Load and Shift Test: Detects excessive translation by assessing humeral head mobility.
5. Therapeutic Implications and Biomechanical Considerations
5.1. Decision-making Based on Biomechanics
- Small lesions (< 13–20%) may be addressed arthroscopically by labral repair and rim fixation.
- Larger defects (> 20–25%) increase recurrence risk unless the bony anatomy is restored via graft or transfer procedures (e.g., Latarjet).
5.2. Goals of Surgical Intervention
- Restore concavity–compression mechanics.
- Increase the articular surface.
- Resecure the negative pressure seal.
5.3. Postoperative Rehabilitation
- Early passive rehabilitation to maintain range of motion without stressing repairs.
- Graduated strengthening to reestablish rotator cuff and scapular control, optimizing biomechanical fulcrums.
6. Long-term Biomechanical Effects
- Persistent Rim Defects: Without correction, can lead to abnormal wear, joint degeneration, and accelerated osteoarthritis.
- Anatomical Restoration: Demonstrated to maintain glenohumeral mechanics and reduce long-term complications.
- Rotator Cuff Compensation: Increased muscular demand can occur if the capsule or rim remains compromised.
Frequently Asked Questions
1. How much glenoid rim loss leads to instability?
Typically, loss above 20–25% significantly disrupts the labral seal and center-of-rotation, creating recurrent dislocations and abnormal joint mechanics.
2. What defines the suction seal in the glenohumeral joint?
It’s a negative pressure chamber formed by the tight-fitting labrum within the socket—when the labrum and rim are intact, this suction effect stabilizes the humeral head.
3. Why use CT scans for glenoid fractures?
3D CT provides exact measurements of fragment size, glenoid version, and bone deficits—crucial for treatment planning.
4. Can the shoulder adapt if part of the rim is missing?
Neural and muscular mechanisms may compensate somewhat, but patients often develop fatigue, pain, and recurrent instability over time without bony repair.
5. What are the goals of restoring glenoid anatomy surgically?
Key aims include reinforcing joint compression, fixing the concavity–compression mechanism, and reinstating the labral seal—to preserve function and prevent arthritis.
6. Are small rim fractures always treatable without surgery?
In select cases involving non-athletic individuals or minimal bone loss, conservative measures (immobilization and therapy) may work. But in most active patients, surgical repair remains the standard of care.
