Advancements in arthroscopic surgery have revolutionized the management of Bony Bankart lesions, offering less invasive options with excellent outcomes. Surgeons now employ specialized suture anchors and refined methods to reattach bony fragments, restore glenoid anatomy, and stabilize the shoulder. This article explores the step-by-step techniques and decision-making involved in arthroscopic repair.
1. Goals of Arthroscopic Repair
- Restore glenoid contour: Reattach displaced fragments to rebuild the glenoid arc.
- Reestablish labral integrity: Secure the labrum to improve stability.
- Preserve bone stock: Use precise placement of anchors to minimize additional bone injury.
These goals aim to reduce recurrence, improve function, and allow athletes and active individuals to return to sport safely.
2. Preoperative Planning
Imaging Assessment
- CT with 3D reconstructions: Determine fragment size and glenoid bone loss.
- MRI or MR arthrography: Evaluate associated labral tears or capsular laxity.
Patient Selection
- Best candidates: Minimal to moderate bone loss (<20–25%), good bone quality, and no significant humeral head defects.
3. Portal Placement and Visualization
Arthroscopic repair requires strategic portal placement:
- Posterior viewing portal: Main visualization site.
- Anterior working portals: Allow placement of anchors and suture passage.
- Accessory portals: Used as needed for specific angles or instrument access.
A clear view of the glenoid rim and bony fragment is essential before proceeding.
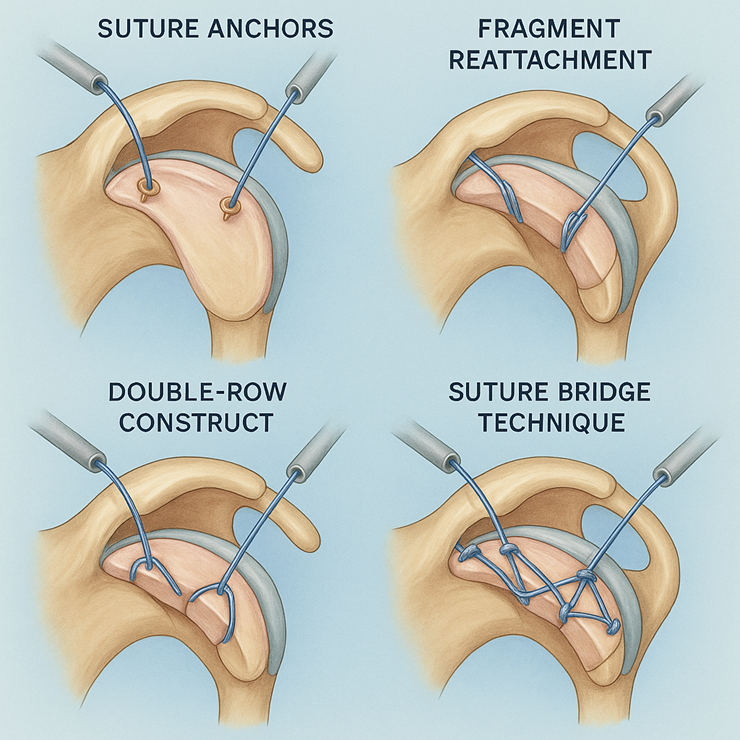
4. Suture Anchor Techniques
4.1 Anchor Selection
- Bioabsorbable anchors: Minimize long-term hardware presence.
4.2 Anchor Placement
- Anchors are placed along the anteroinferior glenoid rim.
- A minimum of 2–4 anchors is typically used depending on lesion size.
- Spacing ensures even tension and stable reduction of the fragment.
5. Fragment Reattachment Methods
5.1 Direct Suture Fixation
- Sutures are passed through the bony fragment and labral tissue.
- Knots are tied to compress and secure the fragment against the glenoid.
5.2 Double-Row Constructs
- Combines medial and lateral rows of anchors to enhance compression.
- Often used for larger or comminuted fragments requiring greater stability.
5.3 Suture Bridge Technique
- Creates a broader compression area across the fragment.
- Useful in fragments with irregular shapes or edges.
6. Rehabilitation After Arthroscopic Repair
6.1 Early Phase (0–4 Weeks)
- Sling immobilization with limited passive range of motion.
- Avoid active external rotation and abduction beyond set limits.
6.2 Intermediate Phase (4–12 Weeks)
- Gradual introduction of active motion and isometric strengthening.
- Focus on scapular stabilization and proprioception.
6.3 Advanced Phase (3–6 Months)
- Progressive strengthening and functional training.
- Clearance for sport-specific activities once full strength and motion return.
7. Outcomes and Considerations
- Success Rates: Arthroscopic repairs show high stability rates in patients with minimal to moderate bone loss.
- Advantages: Less invasive, smaller scars, quicker recovery compared to open techniques.
- Limitations: Not ideal for critical bone loss or severely comminuted fragments.
FAQs
1. How many anchors are typically used in arthroscopic Bankart repair?
Usually 2–4 anchors, depending on the size and extent of the lesion.
2. Can bioabsorbable anchors provide enough stability?
Yes, modern bioabsorbable materials offer strong fixation while minimizing long-term foreign material.
3. What if the fragment is too small for anchors?
Surgeons may opt for labral repair alone or consider bone grafting if instability persists.
4. How soon can patients return to sport after arthroscopic repair?
Most return within 4–6 months, once strength and stability benchmarks are met.
5. Are double-row constructs always necessary?
Not always. They’re reserved for larger lesions or when additional compression is needed. Arthroscopic repair of Bony Bankart lesions combines precision and minimally invasive techniques to restore shoulder stability. Through careful preoperative planning, strategic use of suture anchors, and meticulous fragment reattachment, surgeons can achieve durable results and help patients return to their active lifestyles with confidence.
