The landscape of shoulder instability management is rapidly evolving. With advances in surgical technology, biologic augmentation, and artificial intelligence, the future of treating Bony Bankart lesions promises greater precision, faster recovery, and improved long‑term outcomes. Here’s a look at the innovations shaping tomorrow’s standard of care.
1. Evolution of Surgical Techniques
Minimally Invasive Refinements
- Smaller profile implants: New-generation suture anchors minimize bone disruption while offering strong fixation.
- All‑suture anchors: Reduced hardware footprint with comparable biomechanical strength.
- Arthroscopic navigation systems: Real‑time feedback improves anchor placement accuracy.
3D‑Printed Guides and Custom Implants
- Surgeons can now use patient‑specific 3D‑printed guides to achieve precise fragment reattachment.
- Custom glenoid implants are being explored for complex defects where traditional bone grafts are insufficient.
2. Biologics and Enhanced Healing
Biologic Augmentation
- Growth factors: Delivery of platelet‑rich plasma (PRP) or bone morphogenetic proteins (BMPs) to enhance fragment integration and labral healing.
- Cell‑based therapies: Mesenchymal stem cells introduced at the repair site to stimulate bone and soft tissue regeneration.
Improved Graft Materials
- Use of bioactive scaffolds or collagen matrices in combination with suture anchors to support natural tissue repair.
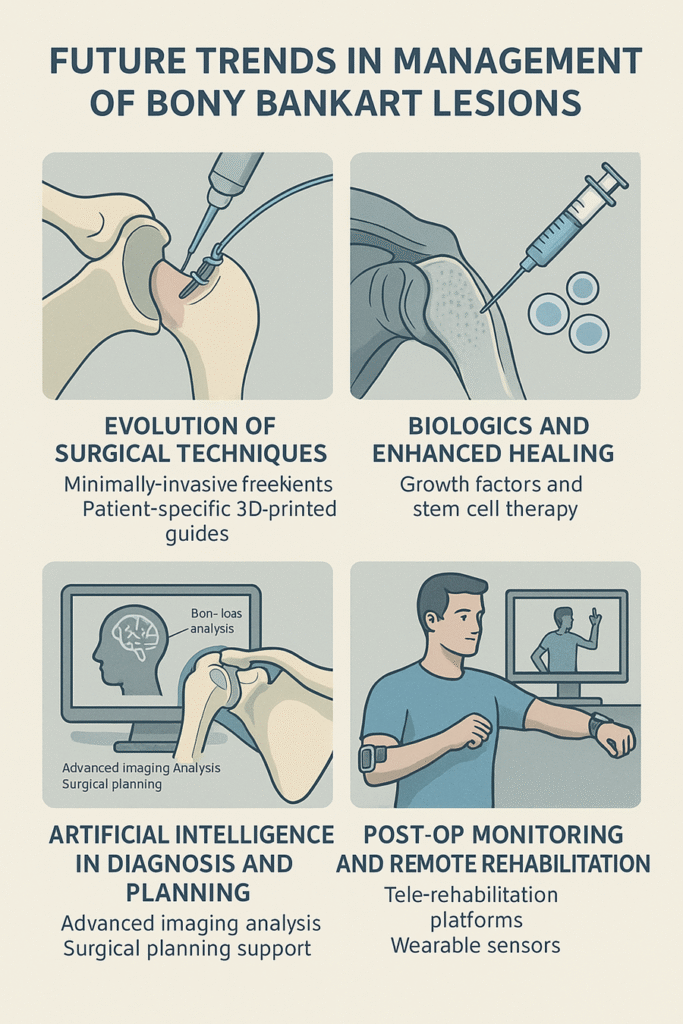
3. Artificial Intelligence in Diagnosis and Planning
Advanced Imaging Analysis
- AI algorithms can automatically identify Bankart lesions and calculate bone loss percentages with high accuracy.
- Predictive models can estimate the likelihood of recurrence based on imaging and patient factors.
Surgical Planning Support
- AI‑driven software integrates patient data to recommend optimal anchor placement or suggest when augmentation is needed.
- Virtual simulations allow surgeons to rehearse complex repairs before entering the operating room.
4. Post‑Op Monitoring and Remote Rehabilitation
- Wearable sensors: Track range of motion, adherence to rehab exercises, and detect early signs of instability.
- Tele‑rehabilitation platforms: Provide guided exercises with real‑time feedback, ensuring patients follow evidence‑based protocols even from home.
5. What This Means for Patients
- Faster Recovery: Less invasive methods and biologics may shorten healing time.
- Improved Outcomes: AI‑guided planning reduces technical errors and enhances stability.
- Personalized Care: Treatments tailored to individual anatomy and risk factors.
FAQs
1. Are all‑suture anchors as strong as traditional ones?
Yes, current research shows comparable fixation strength with reduced bone footprint, making them promising for future use.
2. How soon might biologic treatments become routine?
Some, like PRP, are already used selectively; others are in clinical trials and could become standard within the next decade.
3. Can AI replace the surgeon in planning?
No—AI serves as a powerful tool to assist surgeons, but human expertise remains essential.
4. Will 3D‑printed implants be available for all patients?
Currently, they’re reserved for complex cases, but as technology becomes more affordable, broader use is expected.
5. How can patients benefit from wearable tech in recovery?
Wearables help monitor movement, provide feedback, and detect problems early, improving adherence and outcomes. The future of Bony Bankart management is bright, with innovations poised to make repairs more precise, less invasive, and biologically enhanced. From AI‑powered diagnostics to biologic therapies and custom surgical tools, these advancements promise a new era of personalized care and long‑lasting shoulder stability.
